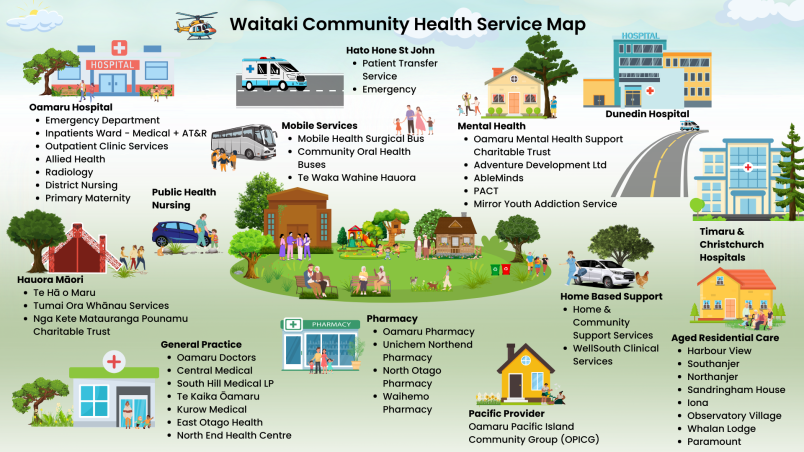
The following information provides a snapshot of Waitaki, its people and health services.
The Waitaki Health Futures Project is looking at ways to improve access and coordination for the services in the following community health service map.
Please note that the above service map is iterative and may be updated over time.
Demographic information: 2023 population data
| Population data: Census 2023 | Total | Māori | Pacific |
|---|---|---|---|
| 2023 population |
23,472 |
2,241 |
1,293 |
| % change since 2018 |
+5.2%* |
+22.9% |
+50.7%** |
| % of population |
n/a |
9.5% |
5.5% |
| Forecast population 2043 |
29,840 |
3,820 |
1,685 |
| Median age |
46.1 years |
27.5 years |
29.5 years |
*Compared to 7% growth in Otago and 6.3% nationally
**The Pacific population was undercounted due to unregistered RSE workers, more people completing the census may account for some of the % increase
***Forecast based on 2018 figures
| 65+ years | 75+ years | |
|---|---|---|
| 2023 population |
5,607 |
2,484 |
| % of population |
23.9% |
10.6% |
| National comparison |
16.8% |
7.3% |
Papatipu rūnanga:
- Te Rūnanga o Moeraki
- Kati Huirapa Rūnaka ki Puketeraki.
Townships include:
- Ōamaru
- Kakanui
- Moeraki
- Palmerston
- Kurow
- Hampden
- Weston
Social indicators
Households: 8,241
Composition: 60% couples without children
Ownership: 56% own their own home
Unemployed: 2.4% (4% nationally)
Employment type: Manufacturing (11.5%), Agri forestry & fishing (7.7%), retail trade (6%), health care & social assistance 5.2%
Median income: $38,430 compared to $42,695 for Otago and $31,800 nationally
Socioeconomic Deprivation Indicators: Waitaki 4.6/10 compared to Otago 5.8/10 (1 = low deprivation, 10 = high deprivation)
Health Status Snapshot
Leading causes of avoidable death:
- Ischaemic heart disease
- Suicide & self-inflicted injuries
- Lung cancer
- Chronic obstructive pulmonary disease
- Cerebrovascular
Māori rates are ~2x higher than non-Māori (Source: Te Tauraki (Ngai Tahu) population data)
| Māori | Non-Māori | Difference | |
|---|---|---|---|
| Female | 82.8 | 84.1 | -1.3 |
| Male | 79 | 80.6 | -1.6 |
Waitaki health indicators
| Regular smokers | Activity limitations | Immunisation | |
|---|---|---|---|
| All population | 14.8% are regular smokers (13.2% nationally) |
8.8% have activity limitations (6.5% nationally) |
78% of 24 month olds are fully immunised (*3 months data) (78% nationally) |
| Maōri |
28.5% are regular smokers |
9.5% have activity limitations |
- |
| Pacific |
20.9% are regular smokers |
6.7% have activity limitations |
- |
Otago health indicators - all population (Source: New Zealand Health Survey)
-
27.6% are hazardous drinkers (22% nationally)
-
58.8% are physically active (52.2% nationally)
-
43.8% consume adequate fruit and vege (34.9%)
-
64% are overweight or obese (66.3% nationally)
-
16.8% have depression or bipolar (16.4% nationally)
Waitaki Health System Profile Overview
Primary and Community
Primary care:
-
GP practices (7)
-
Pharmacies (4)
Available in the community:
-
Hauora Māori & Pacific partners (see below)
-
Mental Health support services (see below)
-
Home & Community Support Services (HCSS)
-
Aged Residential Care facilities (ARC) (6)
-
Rest home level care
-
Secure dementia level care
-
Hospital level care
-
- Public Health Nursing, including
- Sexual health
- Immunisations
- Before school checks
- Education
Oamaru Hospital
Emergency department:
-
24 hr service
-
Fully funded
Outpatients:
- Mixture of public and private outpatient clinics, including:
- chemotherapy and infusion therapy
- Includes outreach from Dunedin Public Hospital
- Face to face and telehealth
Inpatients:
- 20 beds (including Rehabilitaion)
- Stabilise and transfer for paediatrics and high dependency unit
Diagnostics:
- Phlebotomy service
- Awanui Laboratory service onsite
- Radiology, including CT scanner
Allied Health:
- Rehab beds
- Physio
- Dietetics
- Social work
- Occupational therapy
- District nurses
- Speech language
Primary maternity:
- Birthing rooms
- Postnatal beds and care
- Postnatal community care
Hauora Māori services
- Clinical & social services
Tumai Ora Whānau Services – Aukaha Ltd
- Whānau ora navigators
Nga Kete Matauranga Pounamu Charitable Trust
- Smoking cessation services
Pacific health services
Otago Pacific Island Community Group (OPICG)
HNZ funded services
Clinical Services:
- Immunisation clinics
- Screening clinics – Cervical, Bowel screening
- Visiting Clinician support – Dietician, Clinical Pharmacist (Wellsouth supported)
- Pacific Access and Choice Mental Health Clinical Support / Counselling/Family Wellbeing support (partnership with Pacific Trust Otago)
Comprehensive Primary Care Support:
- Health Education and Wellness Support Groups – Kidney support group, Kaumatua stretches group
- Smoking cessation programme
- Kaiawhina and Care Coordination support
- Pacific Access and Choice – 1:1 mental health support/Group wellness and cultural programmes
- Health Promotion Events – Pink Day, Health Expo, Community health campaigns, outreach education support
Other health related services (not funded by HNZ)
Research and insights;
- Health research projects to support Pacific wellbeing
- External health research support in partnership with organisations, government and Universities
Workforce Development and Career Pathways:
- Study Support Hub and pastoral career support for Carers (in partnership with government agencies MSD, MOE and Careerforce)
- Rural placement support for clinicians, Allied health practitioners
Emergency transport and patient services
Hato Hone St John patient services:
- One 24/7 ambulance
- Three volunteer ambulances (Kurow, Palmerston & Oamaru)
- Patient Transfer Service (PTS)
PRIME (Primary Response in Medical Emergencies):
- Kurow and Palmerston
- 7 day a week, 9am-9pm
The PRIME service utilises the skills of specially trained rural GPs and/or rural nurses in areas to support the ambulance service where the response time for assistance would otherwise be significant or where additional medical skills would assist with the patient's condition.
Prehospital emergency care services:
- Two Fire and Emergency New Zealand (FENZ) first response units – Otamatata, Omarama
- Helicopter air ambulance service - delivered by HEMS NZ
Mental health and addictions
Local Waitaki mental health services:
- Integrated Primary Mental Health and Addictions (IPMHA) – Health Improvement Practitioners/Health Coach (HIPS/HC) in GPs (Provider: ADL for Youth, WellSouth for Adults)
- Oamaru Mental Health Support Charitable Trust
- AbleMinds - Supporting Families in mental illness and addiction
- Pact – MH Community Support Worker
- OPCIG – Pacific Access & Choice
Services available out of area, or provided as outreach into the community:
- ADL – Youth Drug and Alcohol counselling
- Mirror Youth Addiction Service
-
Creative Arts Trust (Artsenta) – Day Programme